Dedicated to Our Patients


 Total hip replacement is a common procedure that involves removal of the head of the femur and replacement of the ball-and-socket mechanism of the hip with artificial implants.
Total hip replacement is a common procedure that involves removal of the head of the femur and replacement of the ball-and-socket mechanism of the hip with artificial implants.
As the population ages, this procedure is expected to increase in frequency over the next decade. Patients who undergo hip replacement were typically 60 to 75 years old, and more than 90 percent of hip replacements last 15 years or longer. According to the American Academy of Orthopedic Surgeons the profile of today's replacement patients has shifted from sedentary individual's in their late 60's and early 70's, to active adults in their 50's. Even older patients are remaining more active then previous generations. Improvement of pain and mobility following hip replacement allows patients to maintain independence and quality of life.
Newer techniques, technology (such as computer navigation), and implants have been developed to make hip replacement a less invasive operation, to facilitate recovery time, and to prolong the durability of the implants.
Osteoarthritis of the hip is the most common diagnosis that leads to hip replacement. Osteoarthritis is caused by wear and tear of the cartilage surfaces of the ball-and-socket joint of the hip. As the cartilage wears out, pain and stiffness result. Patients with hip arthritis have difficulty walking, climbing stairs and performing routine daily activities.
Other conditions can also cause destruction of the hip joint, including:
The diagnosis of hip arthritis is made by history, physical examination and x-ray exam. Limitation of motion and pain with motion, abnormal walking patterns and limb-length inequality are commonly seen. X-rays typically show loss of the cartilage space in the hip socket, with a "bone-on-bone" appearance. Bone spurs and bone cysts are also common. Sometimes, additional tests such as magnetic resonance imaging (MRI) or computed tomography (CT) scans are used to confirm the diagnosis.
Although hip arthritis may occur as the result of prior injury or other mechanical abnormalities related to development of the hip, most patients develop arthritis as a result of lifelong wear and tear. Arthritis develops slowly, over a period of years, and gradually becomes more symptomatic with time.
Some bone diseases may contribute to the development of hip arthritis, and patients may also have osteoporosis (brittle bones) in conjunction with arthritis. There is no direct relationship, however, between bone density and the development of arthritis of the hip.
Hip arthritis typically causes intermittent or constant, dull, aching pain in the hip. Patients may feel pain in the groin, thigh and buttock; they also frequently have referred pain in the knee. Walking, especially for longer distances, may cause a limp. Some patients may need a cane, crutch or walker to help them get around. Pain is typically gradual in onset and worsens with time and with higher activity levels.
Climbing stairs can be difficult, so many patients with hip arthritis have to use a stair rail or stop on each step to get up and down. Dressing, tying shoes, and clipping toenails can be difficult or impossible. Pain may occur at rest or interfere with sleep. Rest and use of anti-inflammatory or pain medication can be helpful.
The initial management of hip arthritis includes use of prescription or over-the-counter anti-inflammatory medications such as ibuprofen (Motrin® or Advil®), acetaminophen (Tylenol®), or mild combination narcotics (Tylenol® with codeine). Some nutritional supplements such as glucosamine may also provide some relief. A short-term course of physical therapy may help with strength and stiffness.
For more advanced arthritis, use of a cane in the opposite hand, to transfer weight away from the affected hip, can improve walking ability. A walker may also be used for patients with more severe difficulty walking. These measures usually provide some improvement in pain and function, but arthritis is progressive and worsens with time even with treatment. Weight loss can be helpful to decrease stresses on all of the joints and should also be strongly considered for overweight individuals.
Patients who have progressive problems with pain and mobility, despite appropriate conservative, noninvasive treatment, may be considered for surgery.
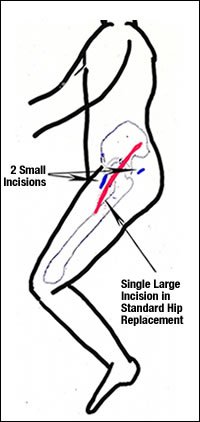
Traditional Hip Replacement: When all of the other measures have been considered or have been tried and failed, hip replacement may be recommended. Traditional hip replacement involves making a 10" to 12" incision on the side of the hip. Muscles are split or detached from the hip and the hip is dislocated. The ball of the femur is removed and the hip socket is prepared by removing any remaining cartilage and some bone to reconstruct the hip socket. Usually, a hemispherical socket is then pressed into the bone of the socket and may be secured with screws. A bearing surface is then inserted into the socket.
Next, the femur is prepared by removing some bone from the inside of the thigh bone and a metal stem is placed into the thigh bone to a depth of about 6". The stem implant is either fixed with bone cement or is implanted without cement. Cementless implants have a rough, porous surface that allows bone ingrowth to secure the implant. A ball is then placed on the top of the stem, and the ball-and-socket joint is recreated.
Minimal Incision Hip Replacement: Minimal incision hip replacement surgery has been developed to allow hip replacement to be performed through one or two smaller incisions. Candidates for these procedures are nearly the same as for standard hip replacement. In Dr. Nessler's practice 90% qualify for the dual incision procedure. The age range he has performed the operation on is 20-96 and up to a BMI of 61. Patients with conditions that distort the normal anatomy or appearance of the bone structures or patients with large bone defects that may require special grafting techniques or implants are frequently not candidates for minimal or muscle sparing hip replacement techniques. The decision to have a minimally invasive hip replacement involves thorough evaluation and discussion with the operating surgeon about risks and benefits. Both traditional and minimally invasive hip replacement procedures are technically demanding and require considerable experience on the part of the surgeon and operating team. At the time of this update Dr. Nessler had performed nearly 1,000 of the dual incision hip procedure.
The artificial implants being used for the minimally invasive hip replacement procedures are the same as those used for traditional hip replacement. Specially designed instruments are needed in order to prepare the socket and femur and to place the implants properly. Implantation of the artificial hip is the same, but the extent of muscle and other soft-tissue dissection is less than with longer incisions.
A single minimally invasive hip incision may measure only 3" to 6", depending on the size of the patient and the difficulty of the procedure. This incision is usually placed over the outside of the thigh.
In the case of muscle sparing techniques (dual incision) the incisions are placed over the front part of the thigh and a smaller incision on the upper buttock region. These incisions will generally measure from 2-4 inches with the smaller 2 inch incision being over the buttock. Muscles are spread apart rather than detached or cut as in the traditional hip replacement operation. This eliminates the need to reattach or repair these muscles to help prevent dislocation of the hip. This is the main reason that patients are able to recover more quickly that in traditional hip replacement and return their normal activities sooner than before. A surgeon experienced in muscle sparing hip replacement technique usually takes no longer to perform this surgery than a traditional hip replacement and will often times require less time to perform this surgery because the extra time needed to repair muscle and soft tissue is not required.
The benefits of less invasive hip replacement are many:
Although early studies suggest that minimally invasive hip replacement surgery is safe,
effective, and streamlines the recovery process, the long-term benefits of this less invasive technique appear to be identical to traditional hip replacement surgery.
Extensive study and development are currently underway to determine the long-term benefits of minimally invasive hip replacement. New technology for imaging and computer-assisted implant placement has been developed and continues to be modified as experience with smaller incision surgery grows. This will allow more precise reconstruction of the hip with less direct visualization. In addition, new implant designs and materials are being developed to both facilitate minimally invasive surgery on the hip and to prolong the lifespan of replacements.
Click here for more information on Direct Anterior Hip Replacement»